Combine the best of artificial and human intelligence
accuracy in data and information extraction
years of IP combined with the latest AI innovations
documents processed
languages supported, empowering customers globally
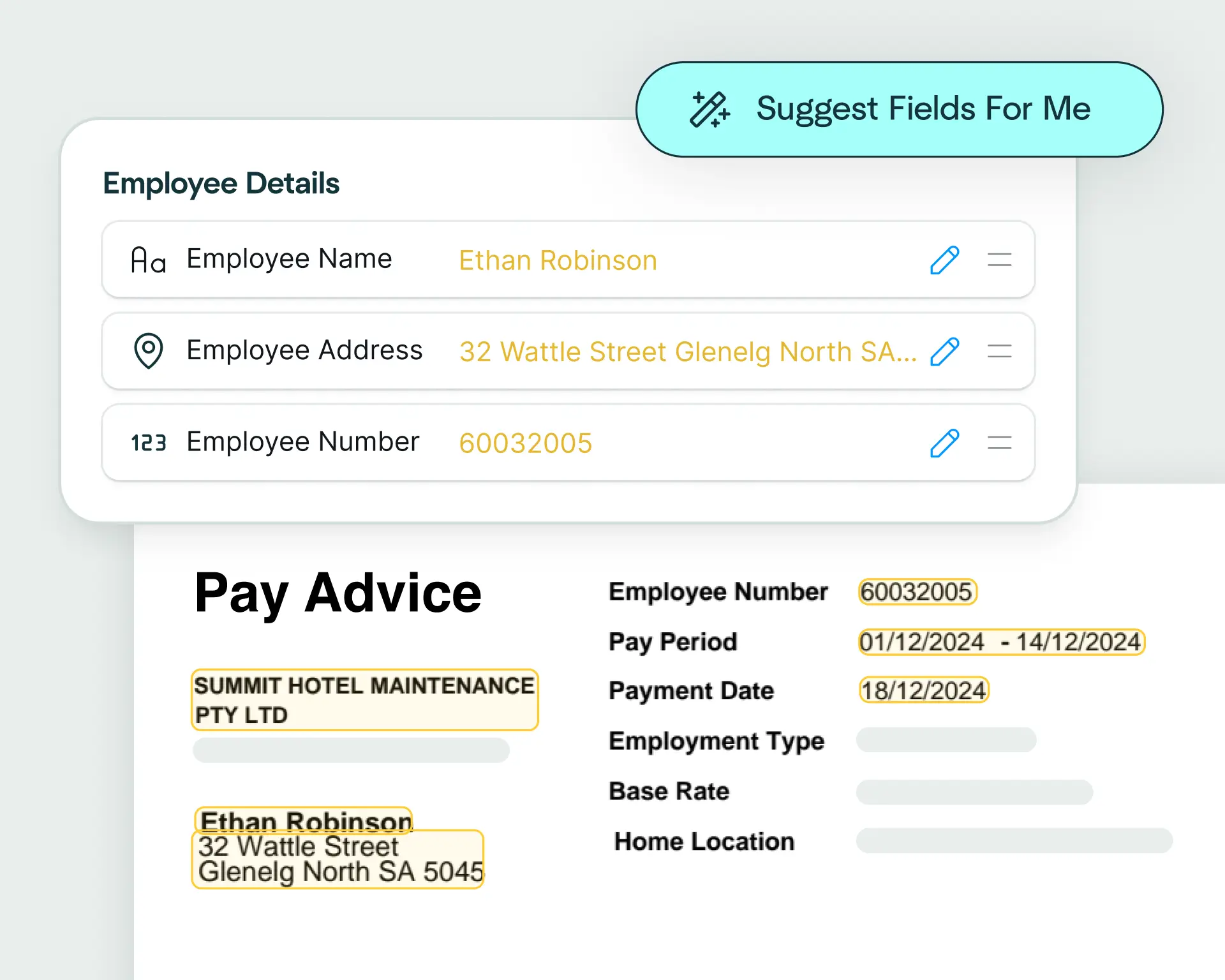
Upload a health insurance claim and watch as Affinda instantly predicts the data fields you need, helping you automate claim data extraction in just a few clicks.
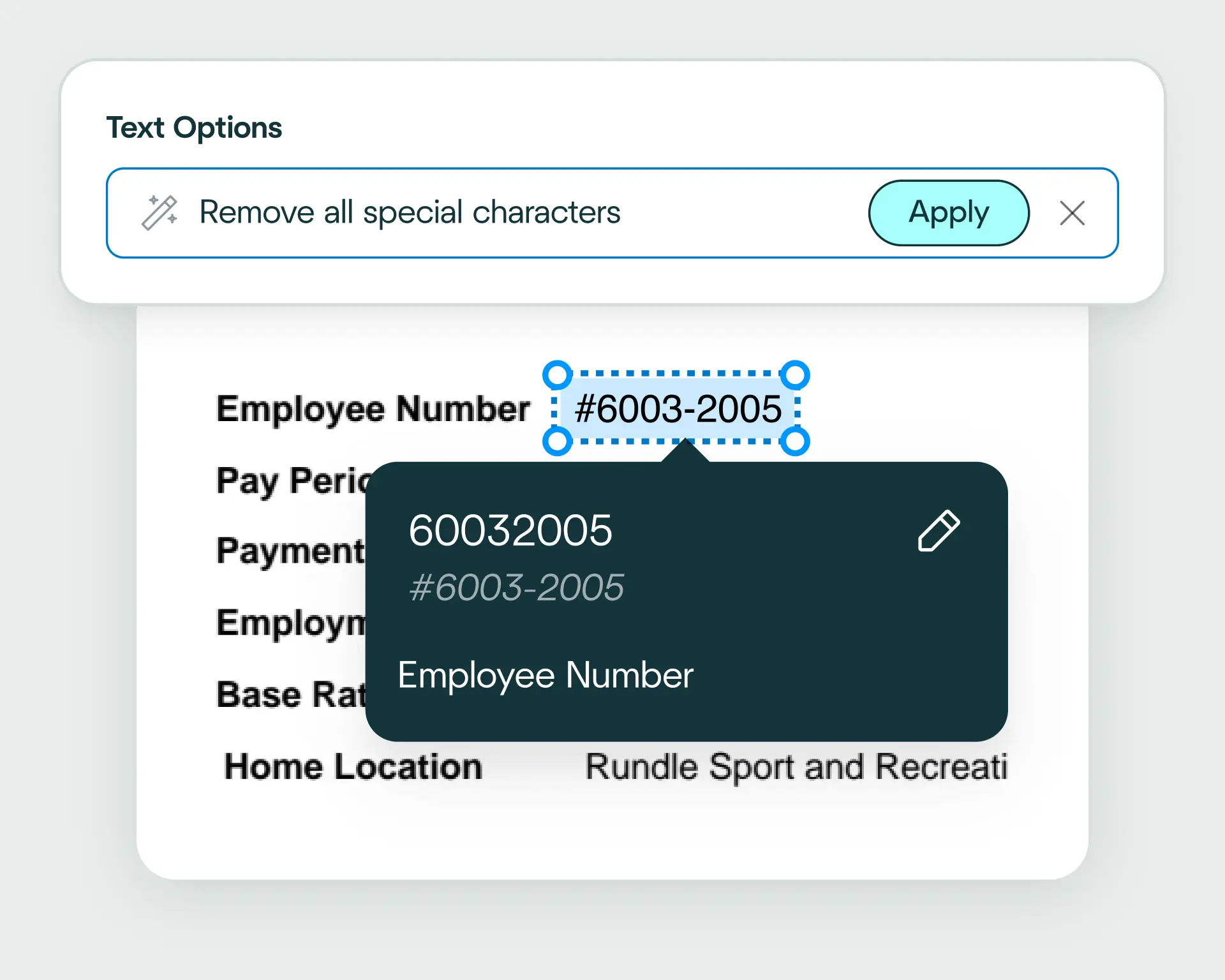
Affinda automatically converts extracted health insurance claim data into the format your claims management or billing system recognizes, ensuring it's ready for immediate use. Need something custom? Use natural language to describe how you want the data structured.
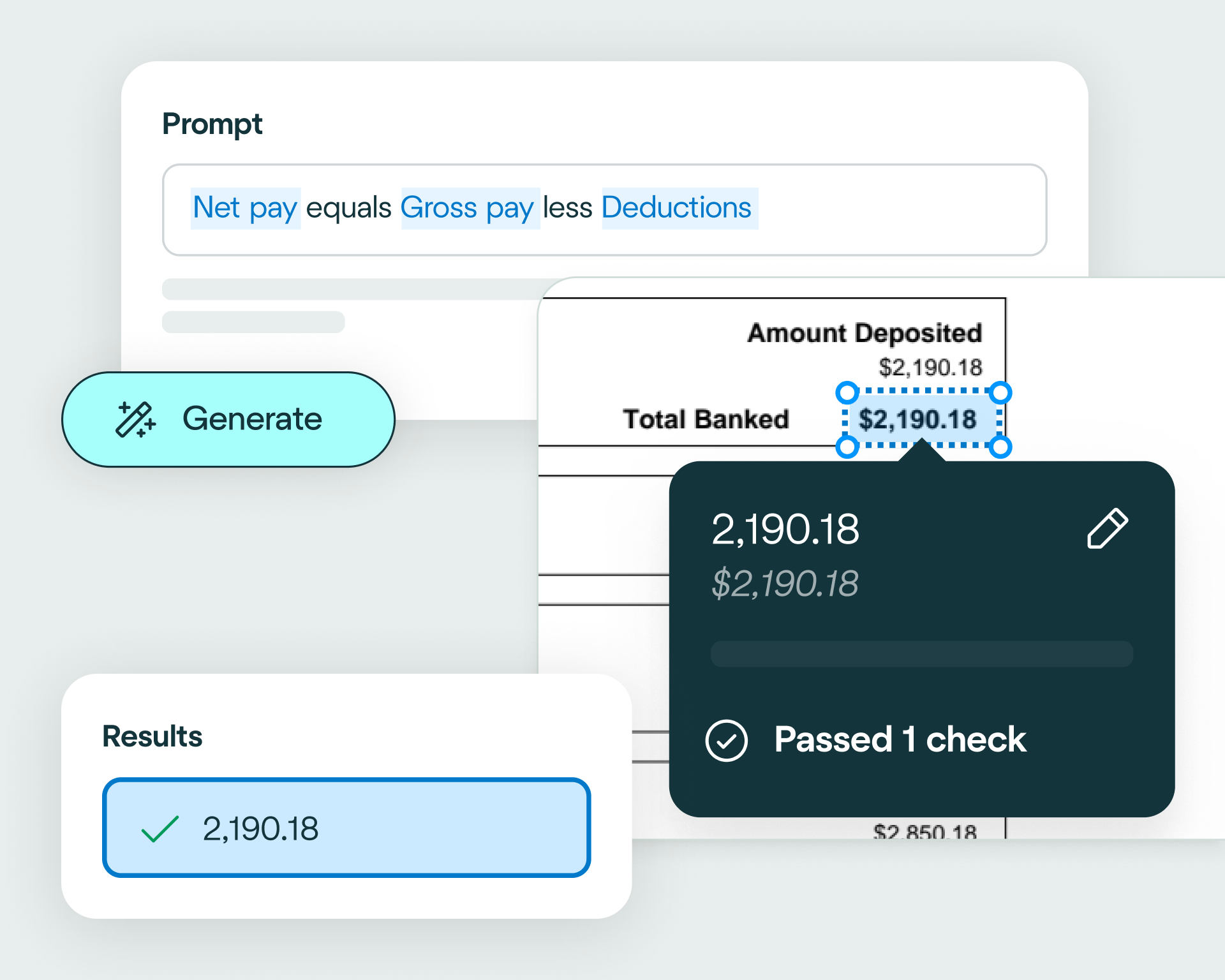
Apply validation rules and business logic to the extracted data, ensuring every health insurance claim meets your accuracy and compliance standards. This enables straight-through processing that reduces manual review.
Create integrations with ease, even if you're not a developer. Choose from 400+ business systems and describe how you want your health insurance claim processing integration to work, using natural language. Affinda's AI Integrations Agent will generate the code to make it happen.
Connect Affinda with your systems using our client libraries. Automatically generate type-safe Pydantic models or TypeScript interfaces tailored to your health insurance claim processing workflows.

accuracy in data and information extraction
years of IP combined with the latest AI innovations
documents processed
languages supported, empowering customers globally
With a free trial, discover how easy it is to extract any information from any document, fast.

Affinda has removed the laborious workload from our accounts staff, who now focus on quality assurance and management of any outliers.
- Nathaniel Barrs, CTO, PSC Insurance
reduction in manual work
more invoices processed with no added staff
Enhanced auditability and tracking of invoice approvals

Customer satisfaction is always our top priority, and Affinda has helped us achieve that by eliminating phone calls, manual handling, and delays.
- Jorg Both, Head of Business Systems, Northline
proof of delivery documents processed annually
of documents straight-through processed in the first weeks
Automatic validation of documents against ERP system

Affinda's ongoing improvements in its AI models demonstrate its innovative approach in Document AI.
– Michael Zhao, AI Product Manager, SEEK

Affinda’s support and expertise were invaluable… The experience working with Affinda was excellent.
- Nick Tran, Business Analyst, StateCover Mutual
documents processed annually
different document types
Enhanced auditability and tracking of invoice approvals

The results have spoken for themselves. I recommend Affinda to anyone looking to enhance their product or business with AI capability.
- Steve O’Keeffe, CTO, Felix
reduction in manual data input
reduction in compliance data errors
compliance documents processed annually
Health insurance claim processing is the workflow healthcare providers and insurers use to receive, extract, validate and approve data from medical claim forms like CMS-1500 and UB-04. Affinda's AI health insurance claim processing software automates this entire workflow – reducing manual effort, speeding up reimbursements and minimizing errors. It ensures claim data is accurate, compliant and ready for your billing, EHR and insurance systems.
Health insurance claim data extraction is the process of reading medical claim forms like CMS-1500 and UB-04 and capturing critical data points – including patient details, provider information, diagnosis codes, procedures, charges and insurance details. Affinda's AI automates health insurance claim data extraction, handling complex tables and multi-page forms to transform unstructured documents into structured data ready for your claims, billing and EHR systems.
Health insurance claim extraction is the automatic capture of key data from medical claim forms using AI. Our health insurance claim extraction software combines reading order models, OCR, LLMs, RAG and more to convert claim information with high accuracy and faster processing times.
A health insurance claim parser is software that automatically reads and extracts data from medical claim forms. It converts claims into structured, machine-readable formats your systems can use. Affinda's AI health insurance claim parser learns from every interaction – adapting to variations in layout, format and custom forms with ease while transforming the output into exactly the format your downstream systems need.
Health insurance claim line extraction captures procedure and charge data from tables within claim forms – turning it into structured, usable data while preserving the relationships between diagnosis codes, procedures and charges. Affinda's complex table capability reads everything from simple grids to multi-line procedure groups, maintaining the connections your billing and claims systems need.
Affinda's AI health insurance claim processing platform can capture data from any field on a medical claim form. Standard data fields include:
Need custom fields or industry-specific data points? Simply define them in the UI or describe them in natural language and Affinda will extract and structure them automatically.
Our AI agents can process any file type. Supported file types include PDF, JPG/JPEG, PNG, TIFF, DOC/DOChealth insurance claim (Word), health insurance claimLShealth insurance claim (Excel), HTML and Thealth insurance claimT/CSV.
Affinda's AI agents read, extract and validate health insurance claim data. Our platform is intuitive to set up and easily integrates into your systems. Simply:
The result? Faster, more accurate health insurance claim processing with minimal manual input.
Yes. Our AI health insurance claim processing platform combines OCR with retrieval augmented generation (RAG), LLMs, agentic workflows, proprietary reading order algorithms and more, to automatically detect and process data from scanned or photographed invoices (PDF, JPG, PNG). Even low-quality images are automatically enhanced for reliable data capture and processing.
Our AI health insurance claim processing platform can automatically detect and process health insurance claims in 50+ languages, including multilingual health insurance claims containing more than one language. Supported languages include: Afrikaans, Albanian, Amharic, Arabic (Standard, Egyptian, Sudanese, Algerian, Moroccan, Levantine), Bahasa Indonesian, Bengali, Bhojpuri, Bulgarian, Burmese, Chinese (Mandarin [PRC/Taiwan], Cantonese, Wu, Min Nan, Jinyu, Xiang, Hakka), Croatian, Czech, Danish, Dutch, English, Estonian, Finnish, French, German, Greek, Gujarati, Hebrew, Hindi, Hungarian, Italian, Japanese, Javanese, Kannada, Korean, Latvian, Lingala, Lithuanian, Macedonian, Malayalam, Marathi, Nepali, Norwegian, Odia, Persian (Farsi), Polish, Portuguese, Punjabi (Western and Eastern), Romanian, Russian, Slovak, Slovenian, Somali, Spanish, Swahili, Tagalog, Tamil, Telugu, Thai, Turkish, Ukrainian, Urdu, Vietnamese, Yoruba.
Yes. Affinda integrates seamlessly with claims management, billing, EHR and insurance systems – plus 400+ other platforms. You can build no-code integrations using our AI integrations agent or connect using our APIs, giving you the flexibility to fit health insurance claim processing into your existing workflow.
AI health insurance claim processing automates and streamlines healthcare workflows across departments such as:
A health insurance claim optical character recognition (OCR) data extractor scans and captures information from medical claim forms such as CMS-1500 and UB-04, regardless of format or layout. Upload claim documents in PDF, JPG or PNG formats. The OCR technology first converts the documents into a text layer, ensuring all text (even from scans, photos or handwritten forms) is captured. Affinda's AI models then identify and extract key fields such as patient details, provider information, claim numbers, diagnosis codes, procedures, charges and insurance details, transforming them into structured, usable data.
This automation eliminates manual data entry, reduces errors and speeds up reimbursements. Once the claim data is captured and structured, our AI health insurance claim processing pipeline can apply business-rule validation and post-processing to enable seamless integration with claims management, billing, EHR and insurance systems.
Healthcare providers, insurance companies and medical billing teams rely on Affinda's AI for their claims operations, revenue cycle management and compliance processes, streamlining workflows and improving overall efficiency.